You test your blood sugar, follow your diet plan, and still wonder, why does it spike after “normal” meals?
Here’s the truth: it’s not the sugar you see that’s hurting your control, it’s the hidden high glycemic index foods you eat every day. That bowl of rice, slice of bread, or morning cereal? They’re working against you faster than you think.
Nutrition experts have pinpointed 20 common foods with a high glycemic index that quietly sabotage diabetes control. Knowing them is the first step toward balanced energy and a calmer glucose curve.
What is the Glycemic Index (GI)?

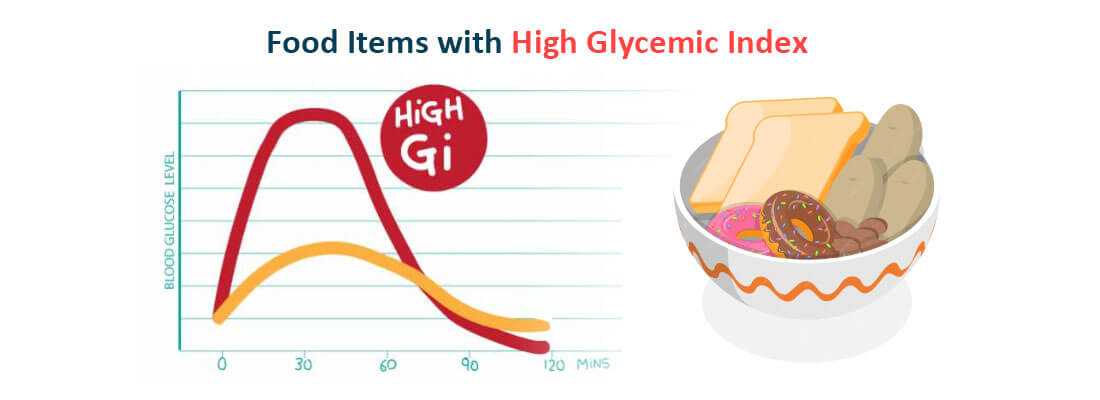
The glycemic index (GI) measures how quickly a carbohydrate-rich food raises blood sugar after eating it, compared to pure glucose, which has a value of 100. Foods are tested under controlled conditions, and their results are plotted on a scale, the higher the number, the faster they raise blood sugar levels.
This measurement is not just about sweetness, it’s about how your body reacts to the carbohydrate structure. For instance, refined foods like white bread or rice are digested rapidly, causing quick spikes, while whole grains or legumes digest slowly, keeping glucose release steady.
Several factors influence a food’s GI value:
-
Type of carbohydrate – Simple carbs like sugar raise GI, while complex carbs digest slower.
-
Fiber content – Foods rich in fiber slow digestion and lower GI.
-
Processing and ripeness – The more processed or ripe a food, the higher its GI.
-
Cooking methods – Boiling or mashing can increase GI, while minimal cooking keeps it lower.
“Managing blood sugar starts long before medication, it begins with what’s on your plate.” — Dr. David Ludwig
Understanding GI helps you plan meals that keep blood sugar stable and energy consistent throughout the day. Once you grasp how it works, you can begin connecting it to broader patterns like glycemic load and food categorization, the next step in decoding how your diet affects blood sugar control.
Track your daily meals smarter with Balanced Bite, your pocket-friendly way to monitor GI and GL in real time
The Relationship Between Glycemic Index and Glycemic Load
The glycemic index (GI) and glycemic load (GL) work together to show how different carbohydrates affect the body’s blood sugar levels. Research in Diabetes Care and J Acad Nutr Diet reveals that both GI values and dietary glycemic index influence energy response.
For example, watermelon has a high GI but a low GL because it contains very little carbohydrate per serving. On the other hand, white rice has both a high GI and GL, meaning it raises sugar levels quickly and significantly.
To understand them in practice:
-
GI focuses on speed — how rapidly glucose enters your bloodstream.
-
GL measures intensity — the total glucose impact from the food’s portion size.
-
Both matter equally for managing diabetes, energy consistency, and preventing sudden sugar crashes.
In simpler terms, GI explains the rate, GL shows the effect. Balancing both ensures you choose foods that release energy slowly and sustainably.
“It’s not just how fast sugar hits your blood, but how long it stays there.” — Dr. Jennie Brand-Miller
This understanding bridges the gap between knowing numbers and using them effectively, which brings us to how the glycemic index chart categorizes foods in real-world eating patterns.
Understanding the Glycemic Index Chart and Its Categories
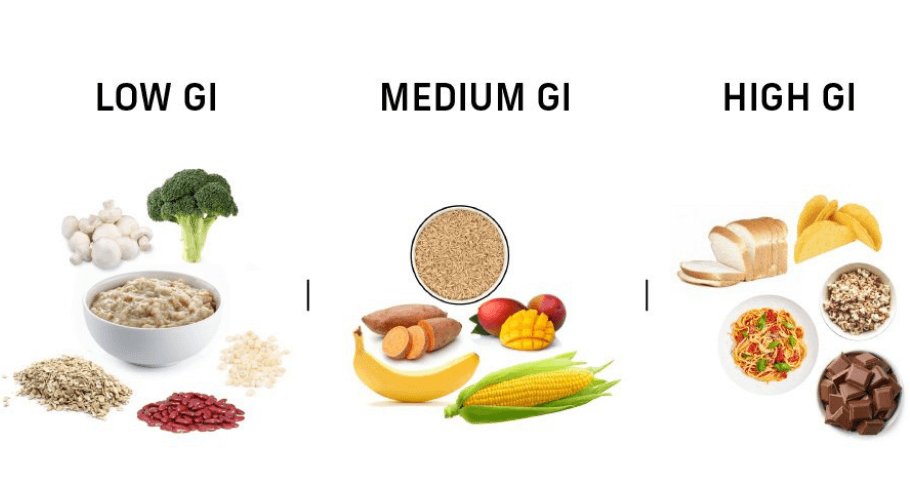
The glycemic index chart groups foods into three categories: low, moderate, and high glycemic index. Based on J Clin Nutr research, these categories reflect how carbohydrates and starchy vegetables affect glucose response.
Recognizing where your favorite foods fall on this scale makes healthy choices easier and gives structure to how you interpret their effects.
1. Low GI foods (1–55):
These are the steady performers. Foods like lentils, kidney beans, apples, chickpeas, yogurt, and barley digest slowly and release glucose gradually. They keep energy levels stable, reduce hunger spikes, and support diabetes control.
These are best for long-term health and sustainable energy through the day.
2. Moderate GI foods (56–69)
This middle range includes brown rice, sweet corn, whole wheat pasta, and sweet potatoes. They provide balanced energy but can still cause mild sugar fluctuations if eaten in large quantities. Pairing them with fiber or protein lowers their glycemic effect and keeps blood sugar steady.
3. High GI foods (70 and above)
These are the fast burners, white rice, potatoes, white bread, cakes, candies, and sugary cereals. They cause sharp glucose spikes followed by sudden crashes, leaving you tired or hungry soon after eating. Regular consumption raises the risk of insulin resistance and energy instability.
“Not all carbs are villains. The right ones power your day, the wrong ones drain it.” — Dr. Mark Hyman
Each GI range tells a different story about how your body handles carbohydrates. Low GI foods sustain, moderate GI fuels, and high GI overwhelms. To see how this plays out in daily eating, let’s explore the most common high GI foods that spike blood sugar quickly.
High GI Foods List: 20 Common Foods That Spike Blood Sugar Quickly
High glycemic index foods include grains, corn, fruits, breakfast cereals, and dairy products that raise blood sugar rapidly. These food items, such as brown rice, sweet potato, or even french fries, are common in many diets.
Identifying these carbs helps in understanding their role in diabetes and how eating habits influence energy. The list below highlights the most common ones.
1. White Bread (GI ≈ 75)
Fast carbs in white bread break down almost instantly, shooting your blood sugar up before you finish the slice. With fiber stripped away, it gives quick energy and an even quicker crash.
2. White Rice (GI ≈ 73)
Refined white rice digests rapidly, leading to sudden sugar surges. Swapping it for brown or basmati rice helps slow absorption and keeps energy steady.
3. Potatoes (Boiled or Mashed) (GI ≈ 78)
Boiled or mashed potatoes act like pure starch once digested, spiking glucose fast. Letting them cool before eating slightly lowers their glycemic index.
4. Rice Cakes (GI ≈ 82)
Light in weight but heavy on GI, rice cakes digest like sugar. They offer quick fuel but no lasting satiety or balance.
5. Cornflakes (GI ≈ 81)
This breakfast classic hits the bloodstream like candy. High in refined starch, it gives instant energy that fades before noon.
6. Watermelon (GI ≈ 72)
Despite being hydrating, watermelon ranks high on the GI scale. Eat it in small portions or pair with nuts to avoid sharp glucose spikes.
7. Dates (GI ≈ 62)
Dates pack natural sugar that digests fast, offering an energy rush that fades just as quickly. A good choice before workouts, not after meals.
8. Doughnuts (GI ≈ 76)
Refined flour, deep frying, and sugar coating make doughnuts a triple threat for blood sugar. They’re dessert disguised as breakfast.
9. Waffles (GI ≈ 76)
Crispy, sweet, and full of refined carbs, waffles release glucose fast. Adding protein-rich toppings like yogurt can slow the impact.
10. Instant Noodles (GI ≈ 55)
Instant noodles raise blood sugar almost as quickly as soda. Their refined flour and salt-heavy sauces make energy peaks short and uneven.
11. White Pasta (GI ≈ 65)
Stripped of fiber and nutrients, white pasta behaves like sugar once digested. Whole-grain versions provide slower, more stable energy.
12. Pretzels (GI ≈ 83)
Pretzels seem light but hit hard on the GI chart. Their refined carbs cause quick sugar jumps that can leave you hungrier later.
13. Pancakes (GI ≈ 67)
Fluffy but deceptive, pancakes made from refined flour spike glucose and drain energy soon after. Balance them with protein or fiber-rich sides.
14. Muffins (GI ≈ 62)
Store-bought muffins mix sugar, refined flour, and oil — a perfect recipe for glucose overload. They rank among the highest GI baked goods.
15. Soft Drinks (GI ≈ 63)
Soft drinks send pure sugar straight into your bloodstream. One can equals an instant glucose spike followed by a hard energy crash.
16. Candy Bars (GI ≈ 70)
Candy bars deliver sugar and fat in quick doses, flooding the body with short-lived energy. They create more cravings than satisfaction.
17. Crackers (GI ≈ 67)
Refined flour and minimal fiber make crackers fast-digesting carbs. They give instant energy that burns out before your next snack.
18. Pineapple (GI ≈ 59)
This tropical fruit digests quickly and spikes blood sugar fast. Pairing it with protein or yogurt helps moderate its glycemic punch.
19. Sweetened Yogurt (GI ≈ 61)
Most sweetened yogurts hide added sugars that counter their health image. Choose plain or Greek yogurt to keep GI and glucose in check.
20. Cookies (GI ≈ 77)
Refined flour, sugar, and butter combine to create one of the quickest blood sugar triggers. Enjoy rarely, and always in moderation.
These foods might look harmless, but their effect on your blood sugar tells a different story. The problem isn’t just what you eat, it’s how fast your body turns it into fuel.
Recognizing which everyday staples hit the bloodstream hardest is the first step toward balance. The next lies in understanding why they behave this way in the first place.
Wondering how your meals compare? Use Balanced Bite’s GI Tracker to check food scores instantly and plan smarter swaps
Why Some Common Foods Have a High Glycemic Index?
Some foods have a high glycemic index because of their nutrients, quantity, and overall nutritional value. The way carbohydrates are processed and the quality of ingredients also affect blood sugar response and diabetes risk.
By recognizing how nutritional makeup shapes GI, you can make healthier choices and adjust your eating habits accordingly.
Key factors that raise a food’s glycemic index:
-
Refinement and processing: Milling, polishing, or removing the grain’s outer layers strips away fiber and nutrients. This makes glucose release faster after eating.
-
Cooking method: Boiling, mashing, or overcooking breaks down starch into simpler sugars, increasing digestibility and GI levels.
-
Lack of fiber and protein: Fiber and protein slow carbohydrate absorption. When a meal lacks them, glucose enters the blood more rapidly.
-
Sugar and additives: Foods with syrups, sweeteners, or hidden sugars digest quickly, pushing GI values higher.
-
Ripeness and portion size: Ripe fruits and large servings increase sugar availability, making even natural foods spike blood glucose faster.
The science is simple, the more a food is processed or refined, the faster your body converts it into sugar. Understanding this helps you build meals that fuel energy instead of draining it. The next section breaks down eight key ways high-GI foods affect your blood sugar and overall vitality.
8 Ways High GI Foods Affect Your Blood Sugar and Energy Levels?
High GI foods raise blood sugar levels quickly, flooding the body with glucose and leading to rapid energy changes. Excess carbs can affect exercise performance, mood, and diabetes control.
Understanding how eating patterns shape these outcomes helps you balance your healthy diet and energy more effectively. Here’s how these foods influence your daily rhythm.
1. Cause Rapid Spikes and Sudden Drops in Blood Sugar
When glucose enters the bloodstream too fast, it causes a sharp rise followed by a quick crash. This roller-coaster effect leaves you tired and craving sugar again within hours.
2. Trigger Increased Insulin Release and Energy Crashes
High GI foods force your pancreas to release more insulin to manage sugar overload. The quick dip that follows results in post-meal sluggishness and loss of focus.
3. Lead to Cravings and Overeating Later in the Day
Sudden sugar drops after a spike confuse your hunger hormones. You end up reaching for more carbs, creating a repeating cycle of cravings and overeating.
4. Reduce Long-Lasting Energy and Satiety After Meals
Low-fiber, high-GI meals burn fast but don’t sustain energy. You feel full briefly, then hungry again much sooner than expected.
5. Disrupt Metabolism and Fat-Burning Efficiency
Frequent sugar spikes signal your body to store energy instead of burn it. Over time, this slows metabolism and makes fat loss harder.
6. Contribute to Mood Swings and Irritability
Blood sugar fluctuations directly affect serotonin and cortisol. The result is irritability, mood dips, and mental fog that mimic stress.
7. Increase Risk of Insulin Resistance Over Time
Constantly high insulin levels reduce your body’s sensitivity to it. This early stage of insulin resistance sets the path toward type 2 diabetes.
8. Affect Workout Performance and Post-Meal Fatigue
High-GI meals can cause quick bursts of energy followed by sudden exhaustion. Athletes and active individuals feel this most during endurance or recovery phases.
Every one of these effects links back to how quickly your food turns into glucose. To manage this better, the next section focuses on identifying and reducing high-GI foods from your diet using proven, science-backed methods.
10 Steps to Identify and Mitigate High GI Foods in Your Diet

Identifying and mitigating high GI foods starts with learning how to read GI values and interpret data from J Clin Nutr or Diabetes Care. Understanding food items, carbohydrate content, and healthy choices gives a strong base for improvement.
When you know what to avoid, you can start applying smarter low GI diet practices to regain balance.
Steps to Identify High GI Foods
1. Identify High GI Foods Using a Verified Glycemic Index Chart
Use a verified glycemic index chart created from research like Brand Miller JC to identify which foods have a high or moderate glycemic index.
This comparison helps you see how certain carbohydrates affect blood glucose and diabetes control.
Start here to separate low-GI foods from those that raise sugar levels faster.
-
Check the GI of your staple foods against the reference food used in studies (usually glucose = 100).
-
Mark anything above 70 as “limit foods” and plan alternatives.
2. Compare Glycemic Load Values to Understand Real Blood Sugar Impact
Comparing glycemic load with glycemic index gives a fuller picture of how foods influence blood glucose. A fruit or meal with low GI can still have a high load if eaten in excess. This step helps you measure total impact, not just speed.
-
Combine both GI and GL values before deciding portion size.
-
Use GL under 10 as a safe daily target for balanced meals.
3. Flag Common Foods With High Glycemic Index for Daily Awareness
Identifying high-GI examples such as white rice, instant cereals, and sugary snacks increases awareness of your eating patterns. By flagging them, you train yourself to pick slower-digesting foods that stabilize blood glucose.
Awareness makes it easier to form consistent, mindful eating routines.
-
Write a short “limit list” and keep it visible while planning meals.
-
Revisit the list monthly as habits improve.
4. Refer to International Tables for Accurate and Updated GI Data
International tables compiled by experts like Brand Miller JC provide updated glycemic index and load values for grains, fruits, and whole meals. Using these ensures your adjustments rely on verified science.
These tables help you compare local staples with global averages for accuracy.
-
Check new versions yearly since GI data evolves with research.
-
Use them as your baseline for menu planning.
5. Track Blood Sugar Changes to Identify Personal Food Triggers
Your body’s response can differ even for the same food. Tracking readings helps reveal personal triggers among high- and moderate-GI items.
By comparing results, you’ll see how specific fruits or meals affect your glucose control and energy differently.
-
Measure sugar one to two hours after eating.
-
Note how long it takes to feel hungry or tired again, that pattern matters.
Steps to Mitigate High GI Foods
1. Replace High GI Staples With Low- or Moderate-GI Alternatives
Swap refined carbs with foods like steel-cut oats, whole fruit, or brown rice. These digest slower and improve long-term glucose balance.
Choosing moderate-GI meals builds a foundation for steady energy without losing flavor.
-
Replace white rice with parboiled or brown rice.
-
Trade white bread for multigrain or rye.
2. Adjust Cooking Methods to Lower the Glycemic Impact of Meals
Cooking style can shift a food’s GI dramatically. Using steel-cut grains instead of instant ones or cooling cooked starches reduces their effect.
This step lets you make healthier versions of everyday meals easily.
-
Light-steam or sauté instead of deep-frying.
-
Chill cooked rice or pasta before reheating to raise resistant starch.
3. Pair High GI Foods With Fiber, Protein, or Healthy Fats to Slow Absorption
Combining high-GI foods with fiber, protein, or healthy fats slows glucose absorption and keeps energy steady.
Pairing fruit with yogurt or nuts turns a quick sugar spike into a balanced meal.
-
Add chia seeds or nuts to fruit bowls.
-
Pair rice with lentils or beans for smoother glucose control.
4. Control Portion Sizes to Manage Total Glycemic Load
Even low-GI foods can raise blood sugar when eaten in large portions. Keeping serving sizes modest maintains stable glucose and appetite.
For instance, a small serving of fruit provides better control than an oversized plate of the same food.
-
Fill half your plate with vegetables, a quarter with protein, a quarter with carbs.
-
Eat slowly to notice fullness cues.
5. Continuously Reassess and Refine Your Diet to Maintain Stable Blood Sugar
Dietary balance evolves with age, activity, and stress. Reassessing intake of low-GI foods and whole grains keeps your sugar curve smooth.
Every small adjustment leads to steadier energy, better diabetes management, and sustainable eating habits.
-
Review your food log weekly.
-
Replace high-GI items one at a time instead of all at once.
Understanding and modifying your glycemic choices isn’t about cutting foods out, it’s about using data, timing, and smarter combinations to make every meal work for you.
Get your personalized low-GI meal guide with Balanced Bite, designed to fit your goals, not restrict your taste
Key Tips for Long-Term Blood Sugar Management

Avoiding all carbs sounds smart until it becomes unsustainable. The real secret to managing diabetes mellitus isn’t in cutting foods out, but in balancing them the same way your body prefers balance, through timing, pairing, and portion control.
“Healthy eating isn’t about perfection, it’s about consistency.” — Dr. Michael Greger
Moderation teaches your body to respond to glucose efficiently while still enjoying healthy foods every day. It’s the difference between short-term fixes and long-term blood sugar stability built on awareness and rhythm.
1. Balance Every Meal Instead of Banning Foods
Combining low glycemic index foods with high-GI ones prevents sugar surges.
-
Pair rice with lentils, or fruits with yogurt or nuts for slower digestion.
-
This pairing extends energy release and smooths post-meal sugar levels.
2. Maintain Consistent Meal Timing
Erratic eating habits strain your insulin response.
-
Eat three balanced meals and one or two light snacks at regular times.
-
Consistency trains your body to use glucose efficiently and reduces cravings.
3. Choose Smarter Swaps, Not Total Elimination
You don’t have to give up your favorites, just modify them.
-
Switch instant noodles for millet-based or whole-wheat versions.
-
Replace white bread with multigrain or sourdough.
-
Enjoy naturally sweet fruits instead of processed desserts.
4. Manage Portion Sizes and Frequency
Even low glycemic index foods can affect sugar balance in large portions.
-
Use smaller plates to reduce intake visually and mentally.
-
Treat high-GI foods as side portions, not the main focus.
5. Move a Little After Meals
Physical activity helps muscles absorb glucose effectively.
-
A 10-minute walk post-meal can lower blood sugar naturally.
-
Regular movement complements dietary moderation perfectly.
6. Stay Hydrated and Manage Stress Levels
Hydration supports metabolism while stress control prevents hormone-driven spikes.
-
Keep a water bottle nearby throughout the day.
-
Practice deep breathing or short meditations to calm cortisol levels.
7. Revisit and Refine Your Eating Pattern Regularly
Your needs evolve, and so should your plan.
-
Review glucose readings and energy patterns every few weeks.
-
Adjust food combinations or portion sizes as your lifestyle changes.
True balance doesn’t come from saying no to food, it comes from knowing how much, when, and what to say yes to. When you eat with awareness, healthy foods become tools for control, not restriction.
Stay consistent, not perfect. Join Balanced Bite today to turn your diet into a lifelong habit of balance
Conclusion
Knowing these high-GI foods is one thing, acting on that knowledge is where real change begins. Start by replacing one refined food on your plate each week with a steadier, low-GI option.
Let your meals work for your body, not against it. The sooner you take charge of your choices, the faster your blood sugar finds its balance.




















Leave a comment
Translation missing: en.blogs.comments.discription